How To Process An Insurance Claim
As a reminder, the following tasks must be completed before you can begin billing insurance using TiQ
- Your company's insurance billing settings must be complete and accurate within your company settings
- The client, associated with the claim being processed, must have complete and accurate insurance information within their client profile
- To receive communications (e.g. ERAs, Verification of Benefits) from the clearinghouse, you must complete the enrollments necessary for the provider.
In TiQ, claims are automatically generated in Insurance iQ with a Pending status once a calendar event is marked as attended. Please note that claims are only created for clients who have active insurance information entered in their profile.
NOTE: Additionally, depending on your claim generation settings, a completed progress note may also be required in order for a claim to be generated. Click here for additional information on how to configure claim generation
The following guide will walk you through the steps to process a claim in pending status:
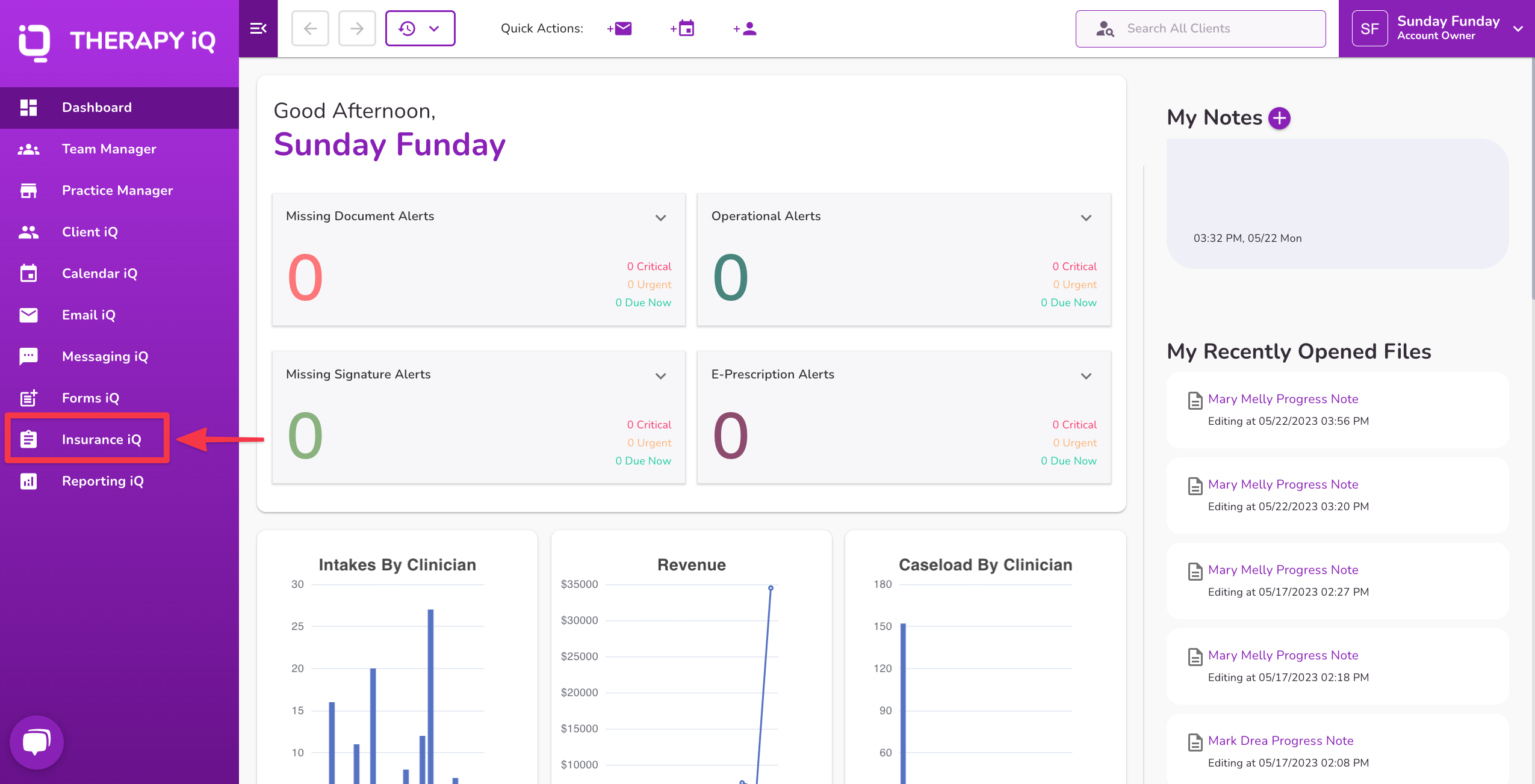
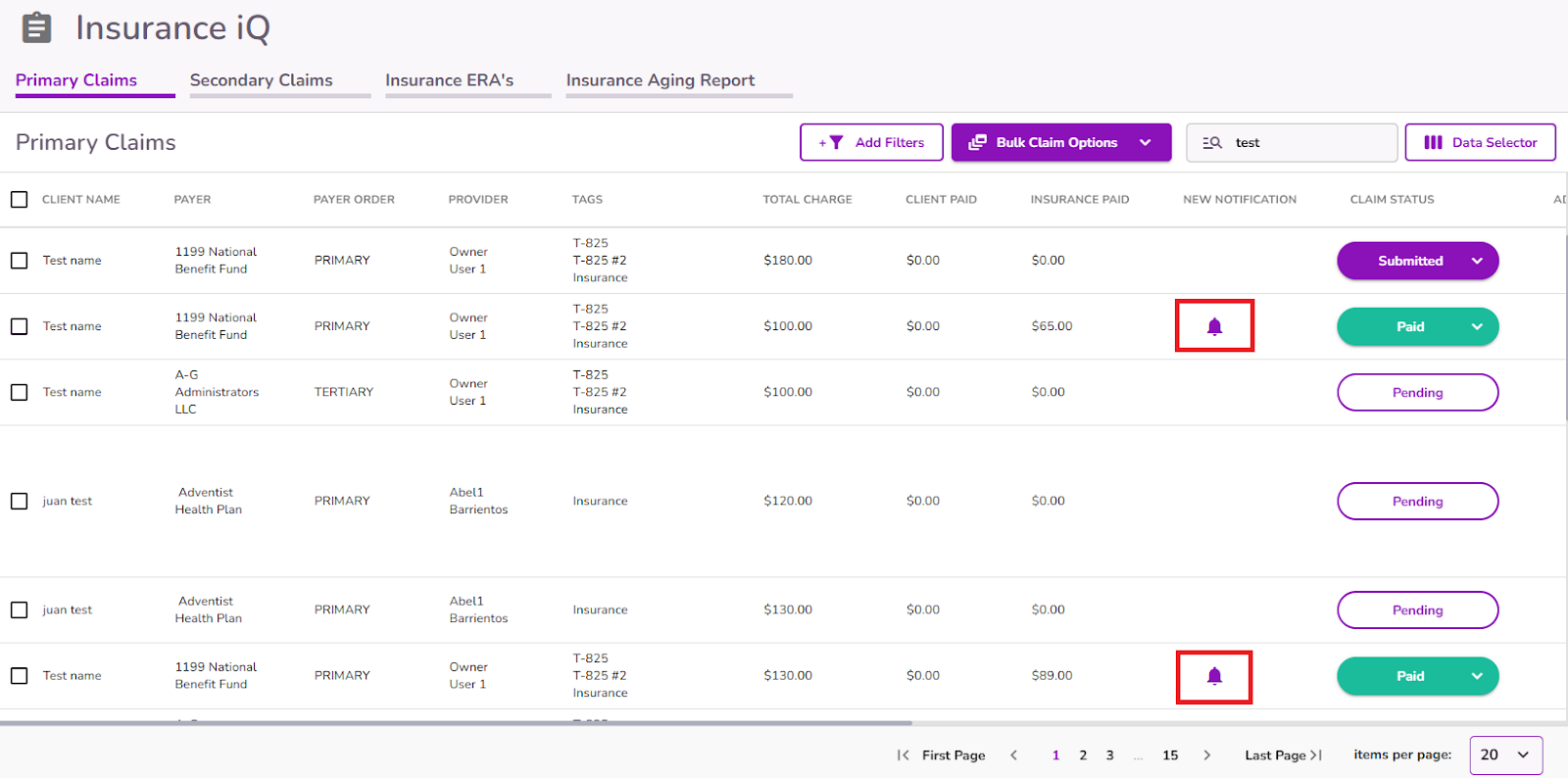
From the Navigation Bar, navigate to Insurance iQ, and then select Insurance Claims
This log will contain all claims that have been generated based on appointment attendance marked "Attended" and Insurance Info being present in a client's file.
NOTE: The status of claims will update based on whether they have been submitted and the response received from the clearinghouse or the appropriate payer.
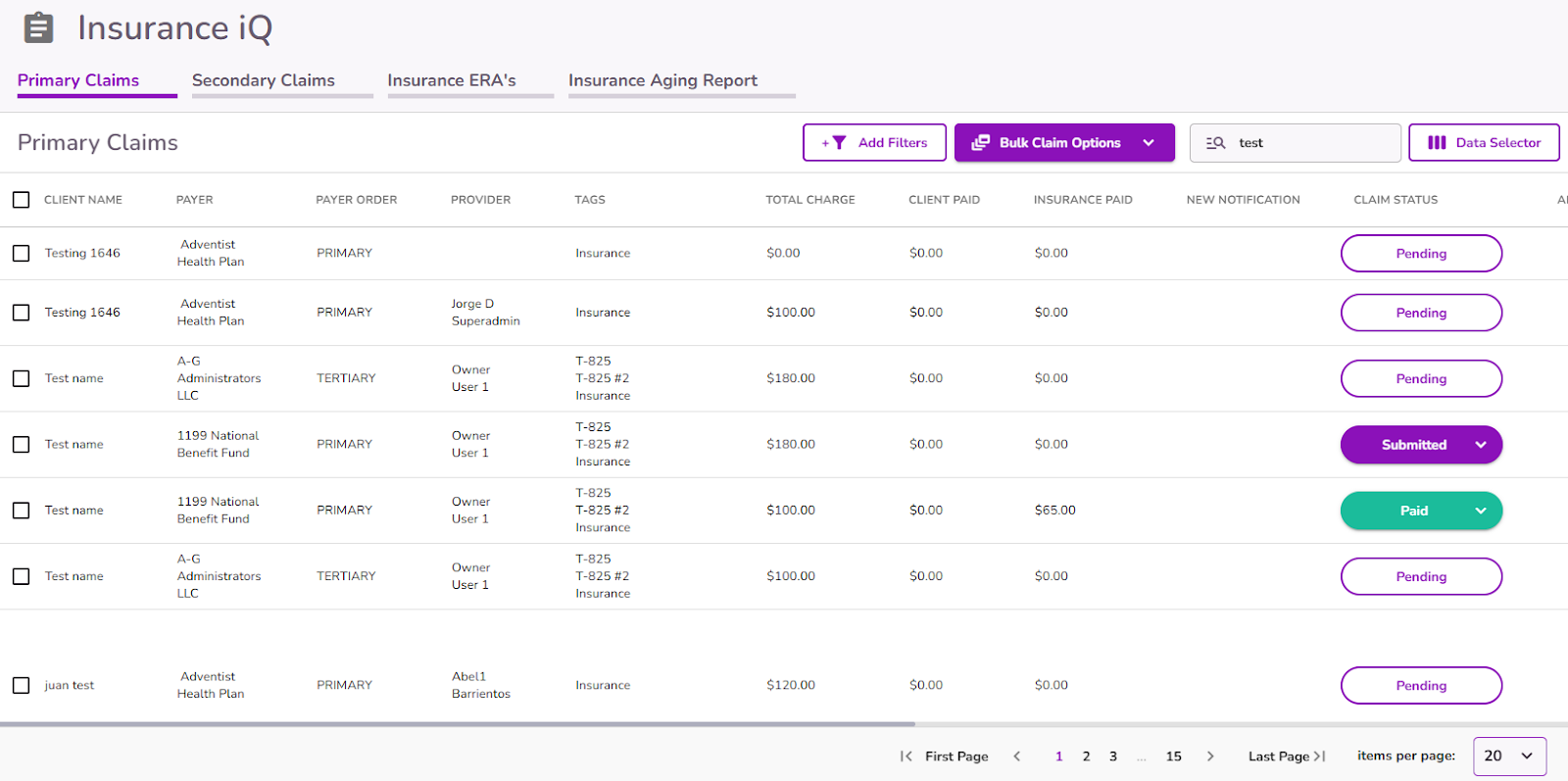
Click here for additional information on claim statuses
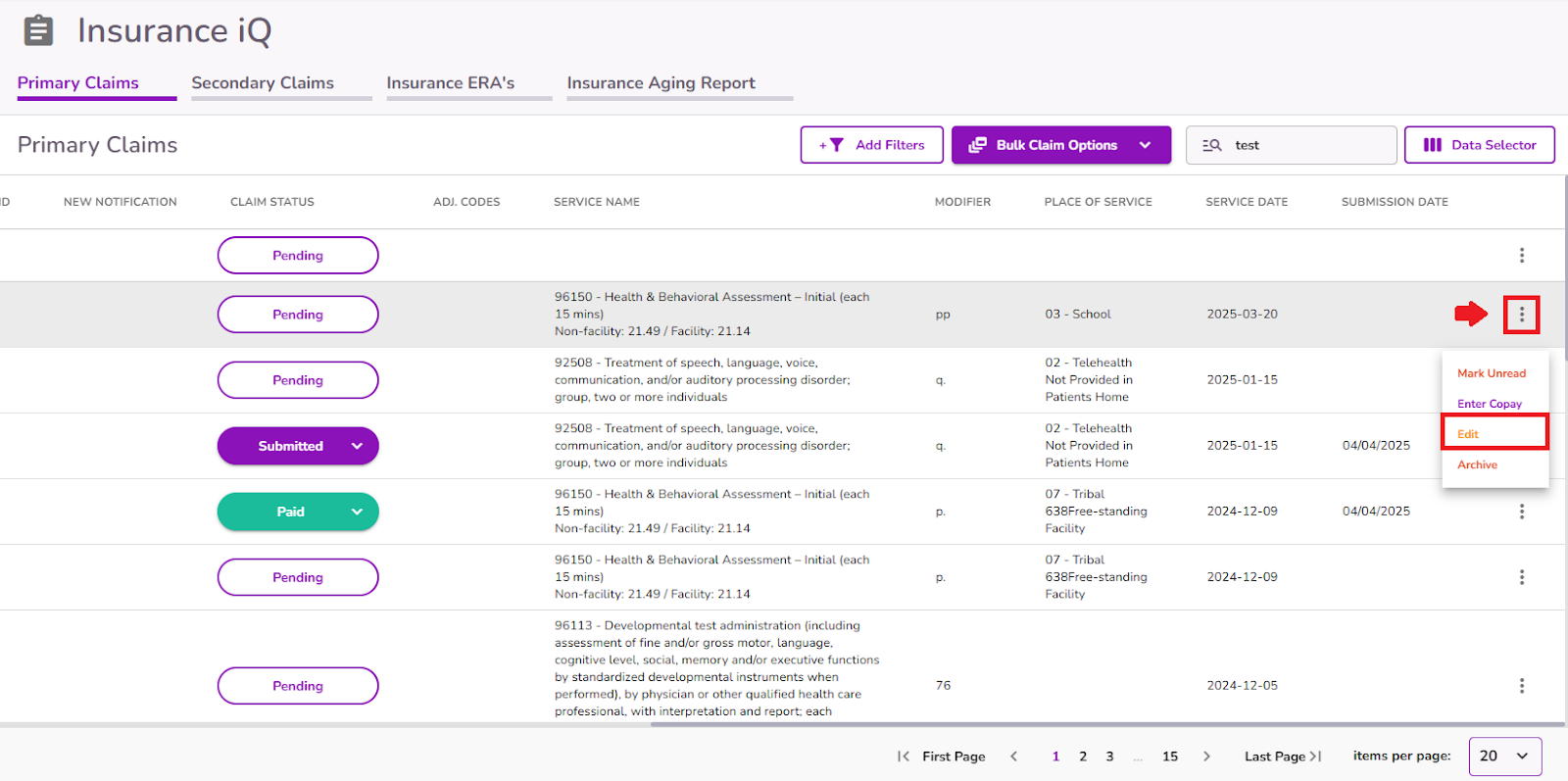
To process a claim in Pending status, locate the corresponding claim in the list and either click directly on it or select the three dots next to the claim and choose Edit.
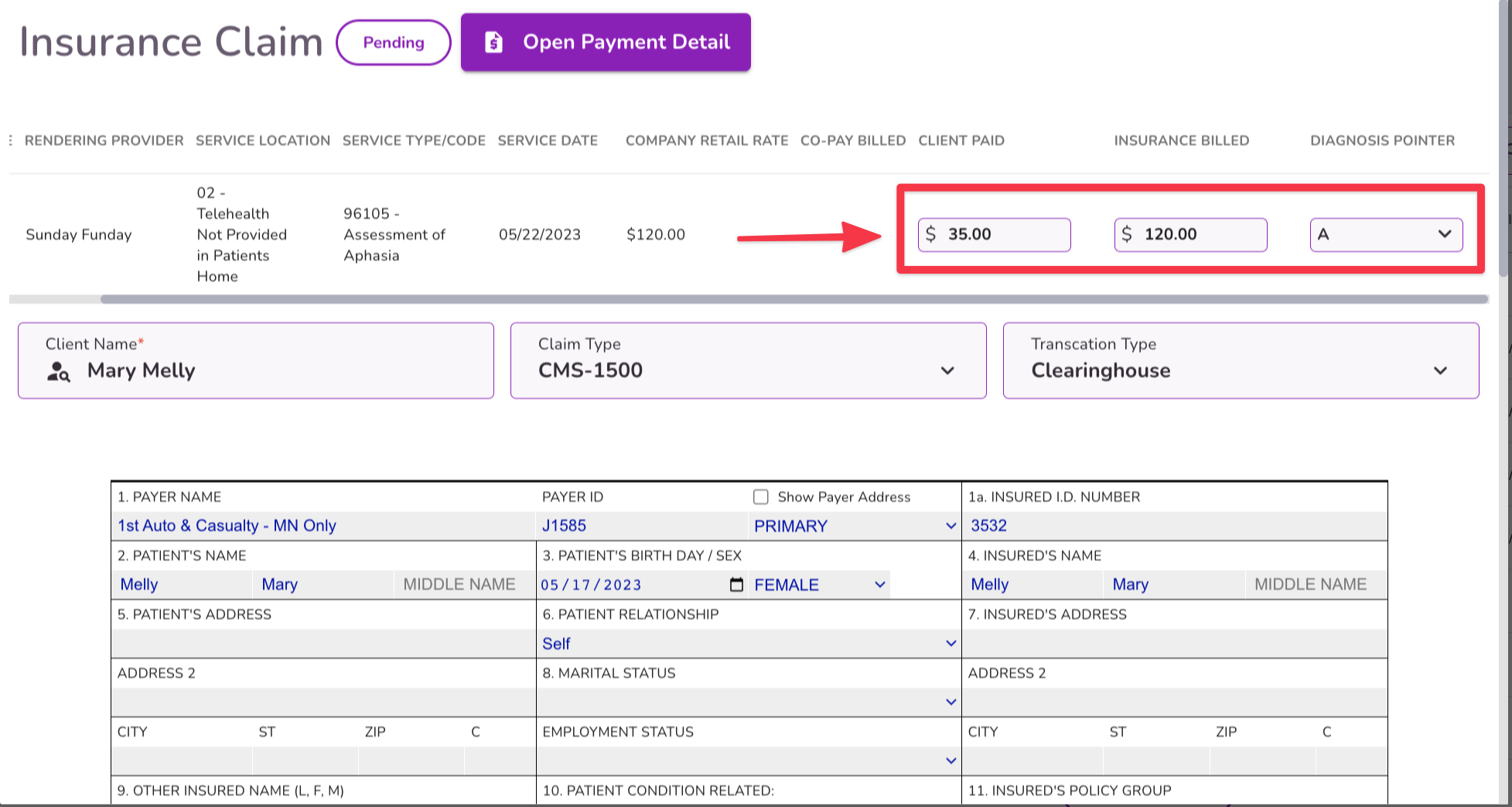
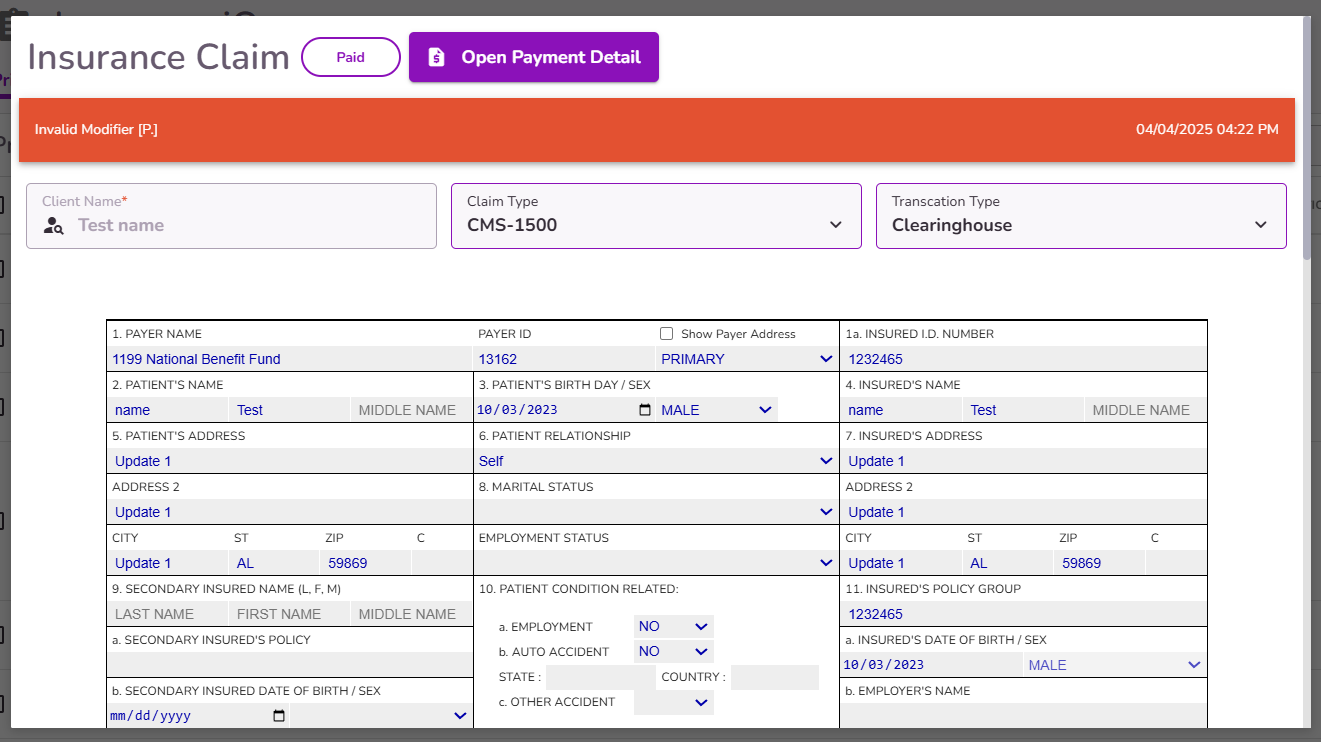
Insurance Claim Form
The claim form will appear, displaying the automatically populated fields. You can review, modify, or manually enter any additional information as needed.
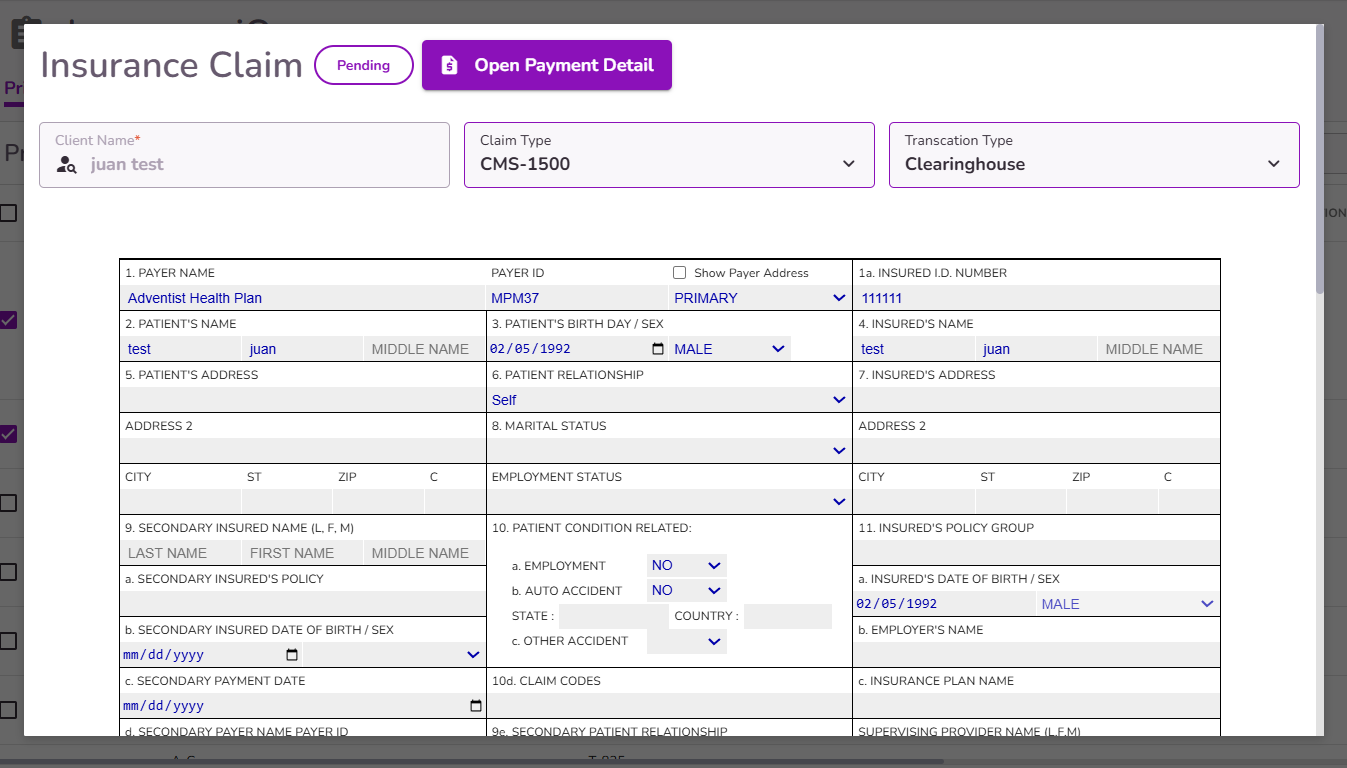
If the claim is pending submission, complete the following steps to submit the claim:
Ensure that the diagnosis pointer is referencing the correct code in field 21 of the claim form (This is autofilled from your clients profile page.)

The Claim type & Transaction type will auto fill. Update if necessary.

If any payment towards this service has been collected from the client from the calendar event, you will see this autofilled here.
For new generated claims, Box 22 will display the '1 – Original Claim' option selected by default.
When an ERA is received for a specific claim, Box 22 will be updated with the appropriate option and the PAYER ICN.
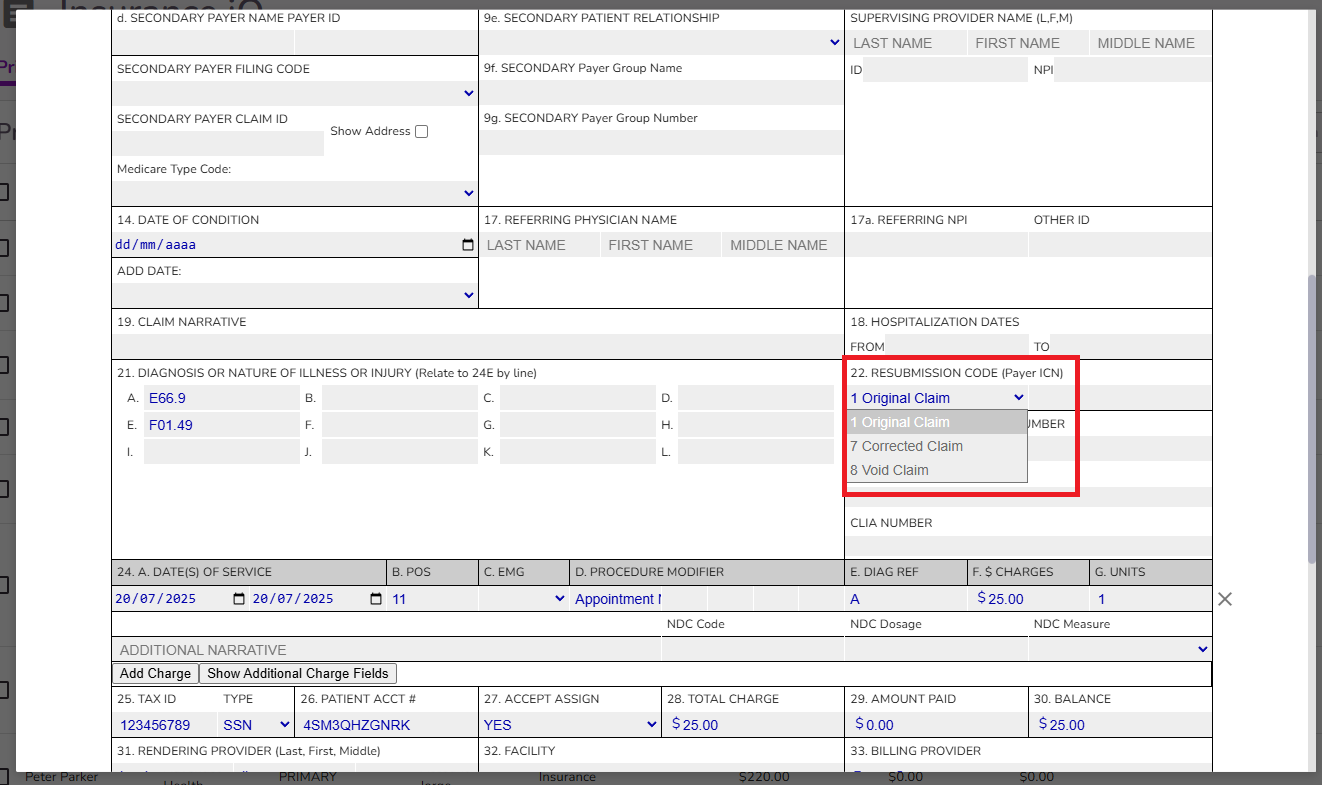
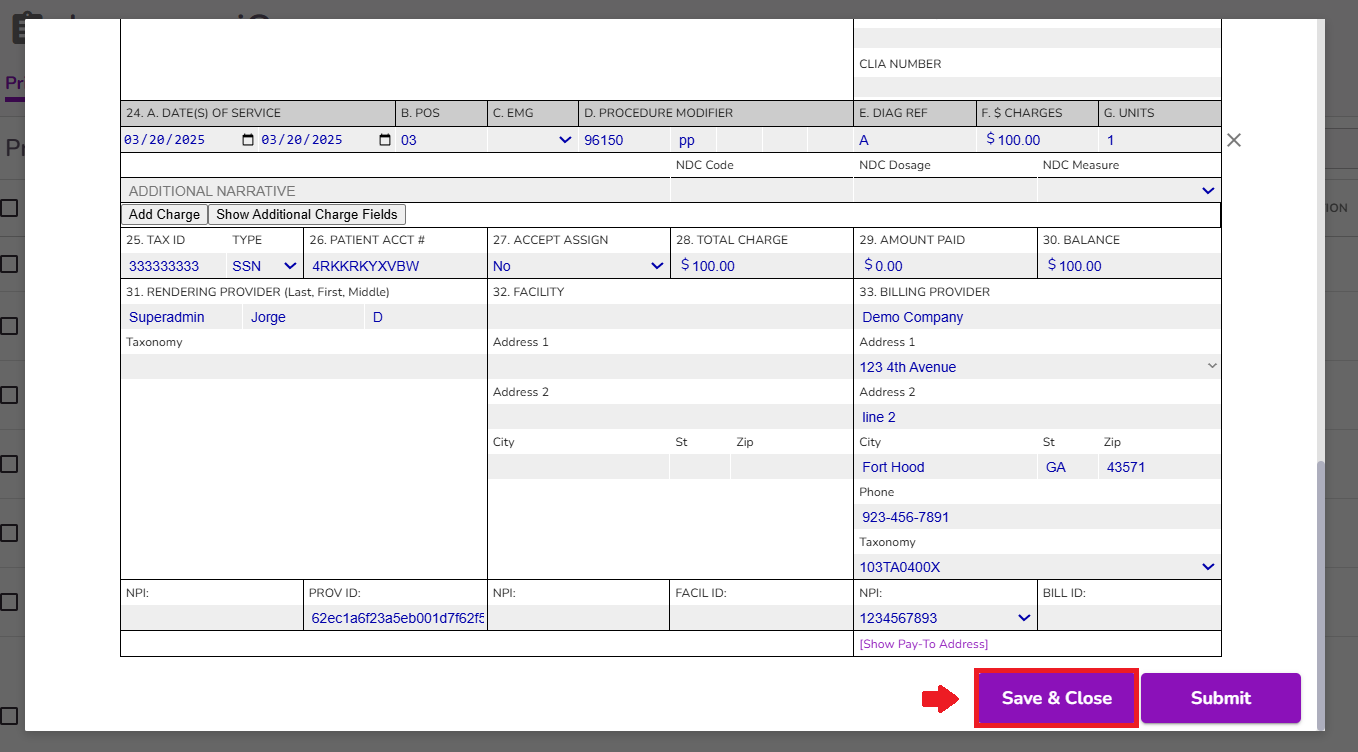
The details from section 24 will autofill from your calendar event.
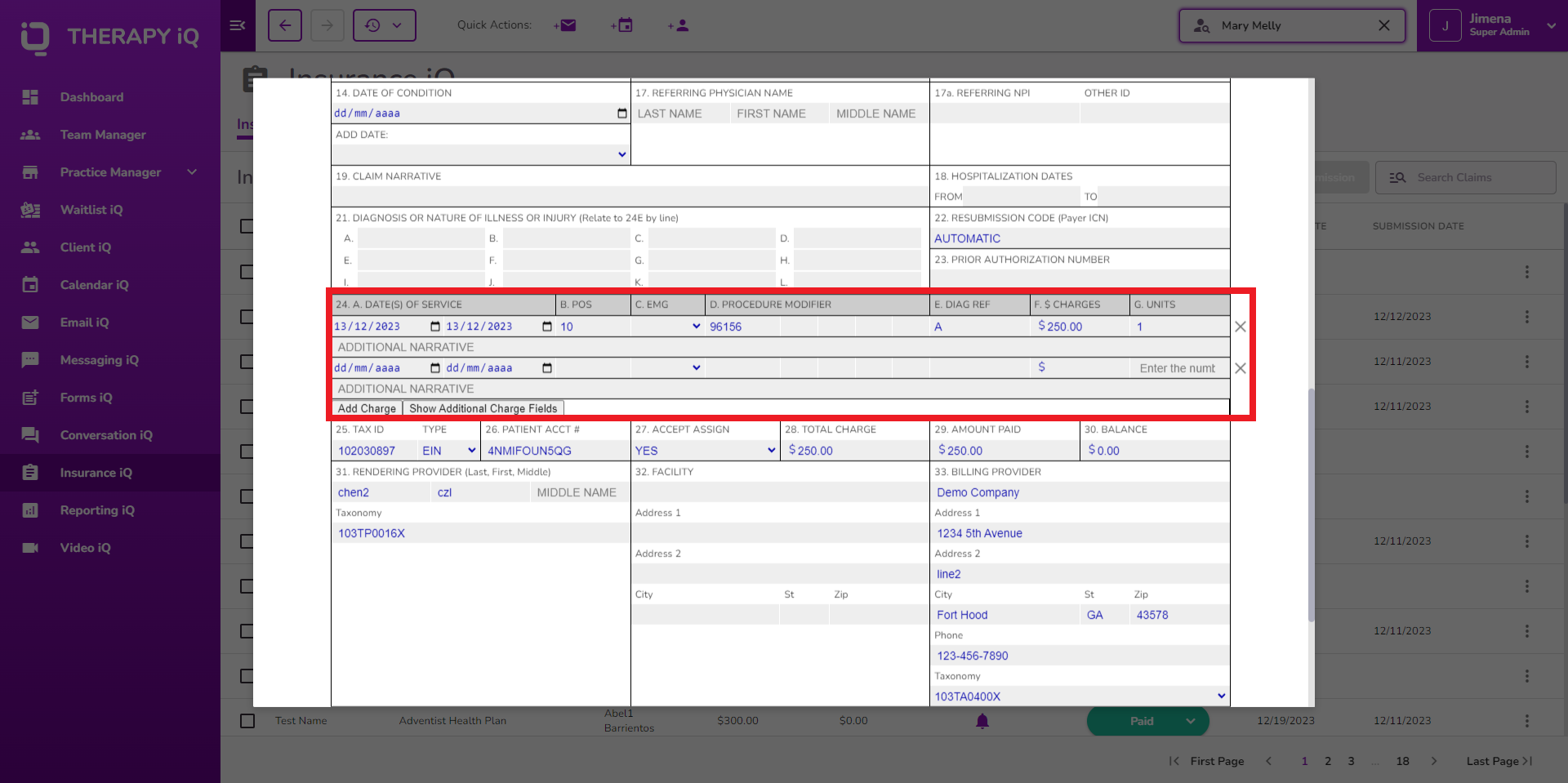
NOTE: If you add a charge with the 'Add Charges' button the information added will update the calendar event, update the invoice, and update the ledger.
If the claim has been submitted, and then then you and add charges, this will update the claim, invoice, ledger.
You can only enter additional dates with the same service date.
Submit
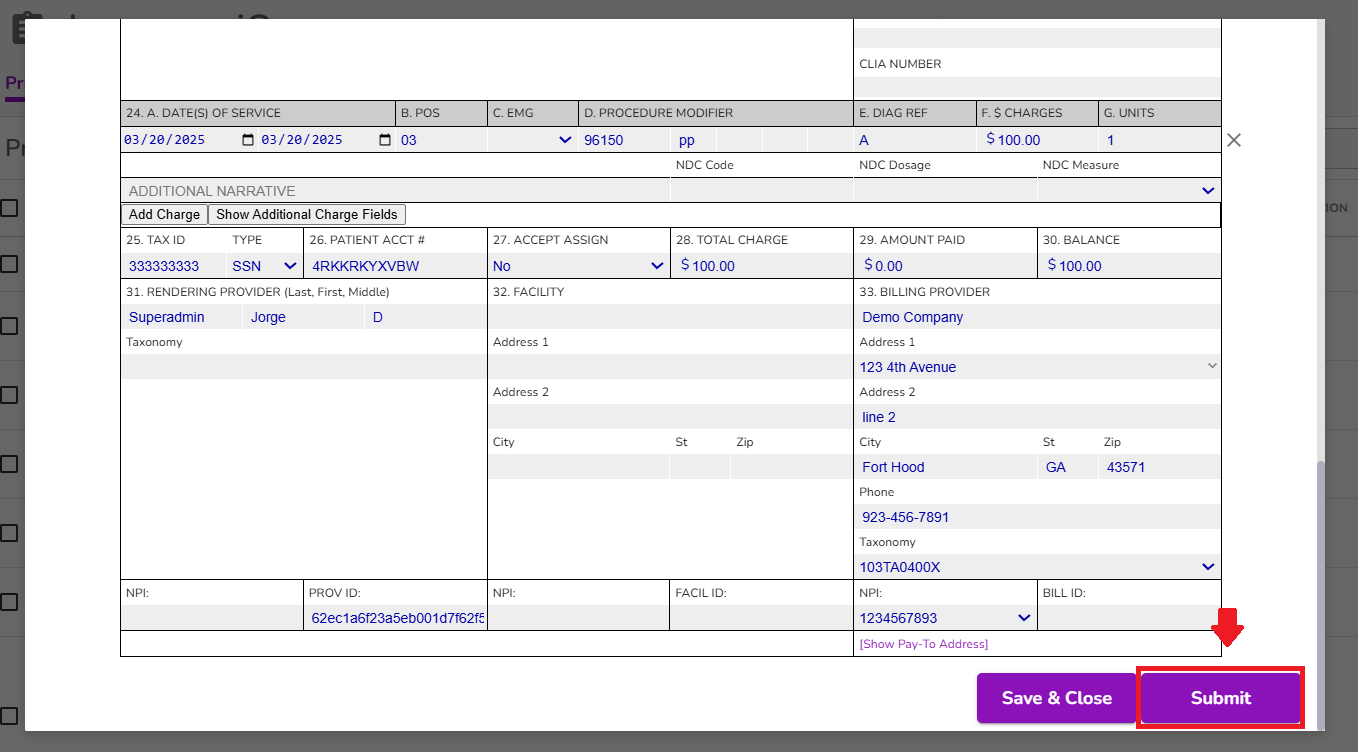
Once the claim is submitted, its status will automatically update to Submitted or Rejected, depending on the information entered and the response received from the clearinghouse.
NOTE: You have the option to Save and Close the claim if you prefer to process it at a later time. Any changes made will be saved, and the claim will remain in pending status. You can reopen and submit it whenever you're ready.
Once submitted and a notification returns from the clearinghouse, the new notification column displays a Notification Bell until viewed
Click on the row of the claim you would like to review to view its notifications and take any necessary actions. Any error codes will appear in red at the top, indicating the fields that may require review or correction.
Once the notification has been viewed, the bell icon will be removed
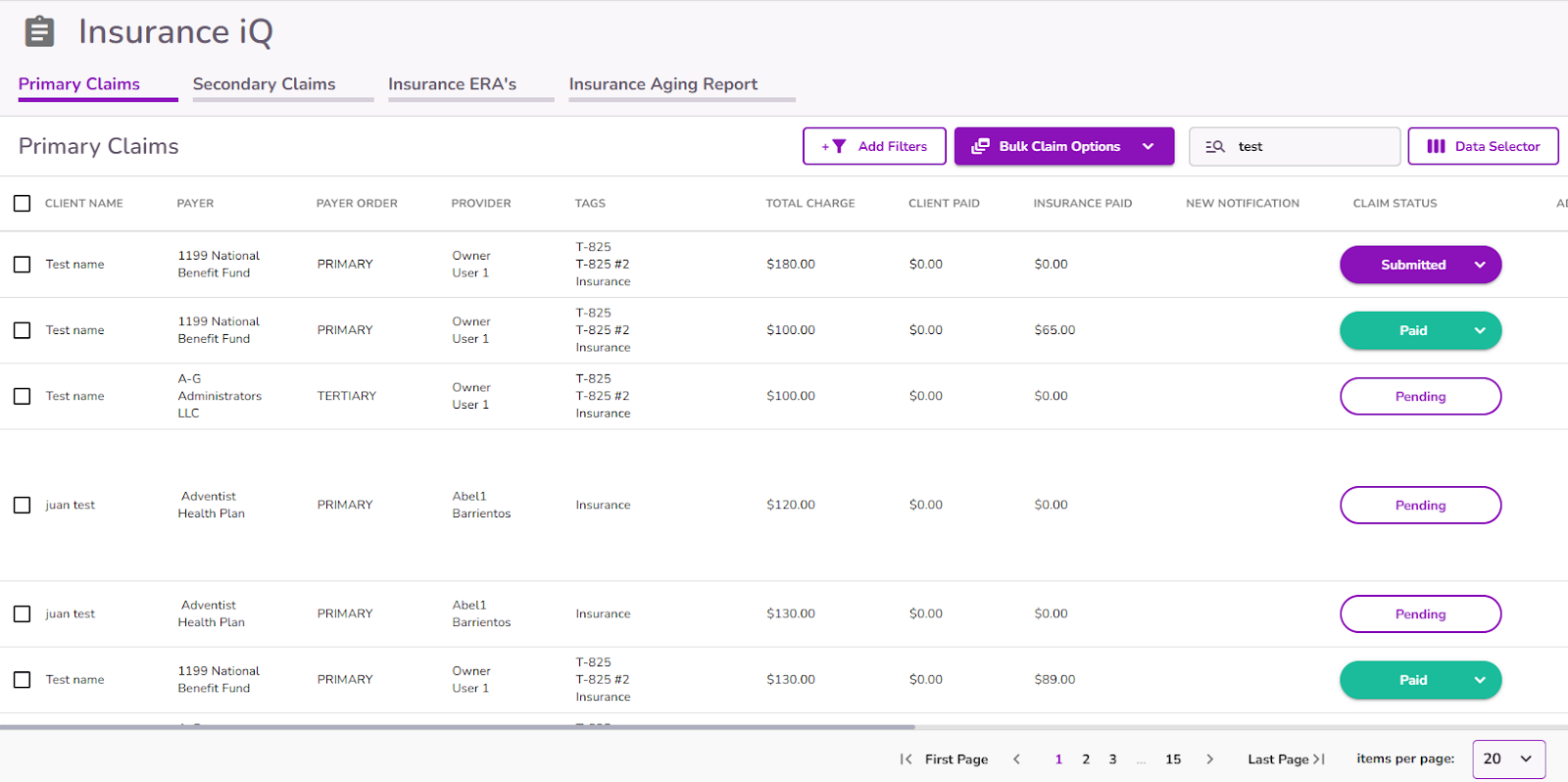
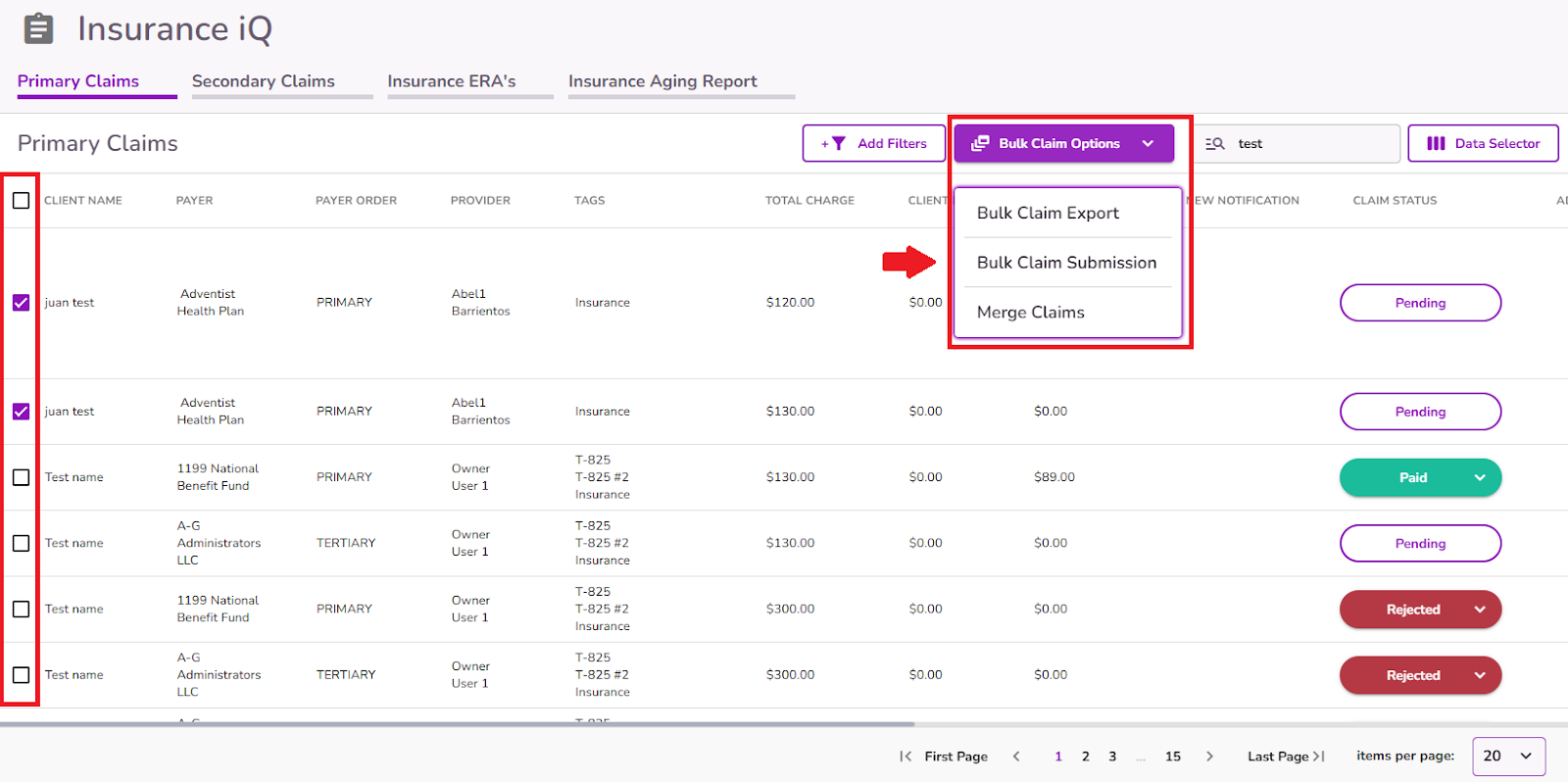
NOTE: If needed, you can use the checkboxes on the left side to select multiple claims and submit them in bulk.
For additional information, please refer to our guides below:



